On average, there are over 6 million passenger car accidents in the U.S. every year. Road crashes are the leading cause of death in the country, resulting in more than 38,000 people losing their lives each year.
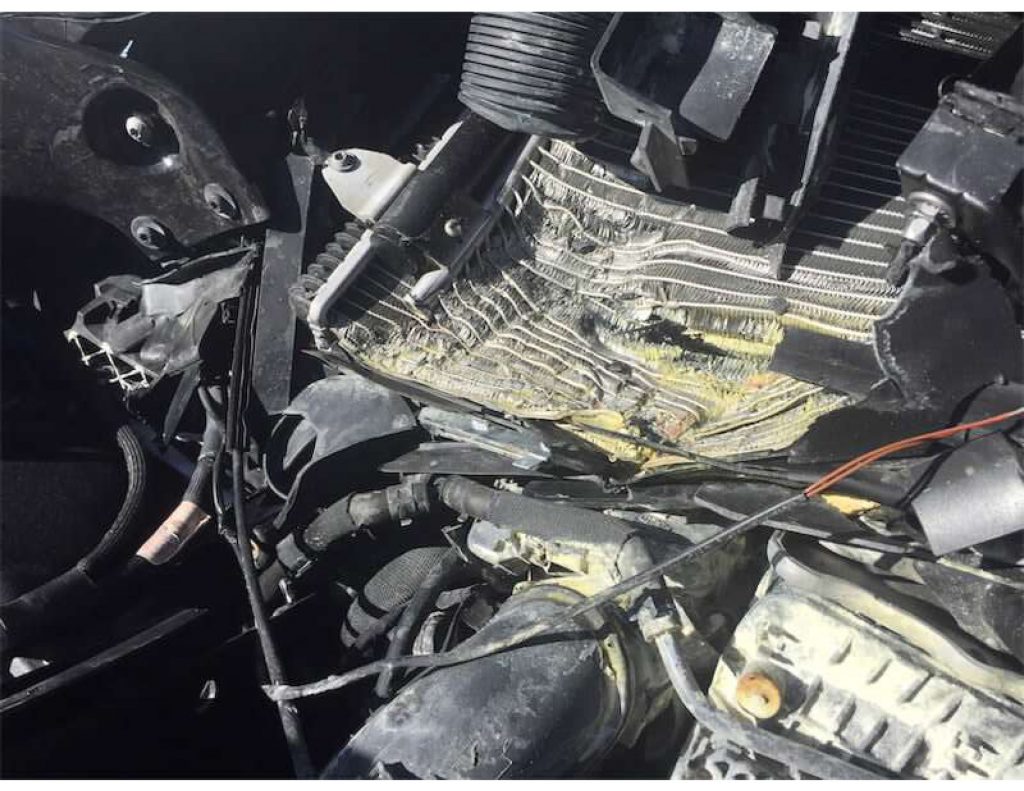
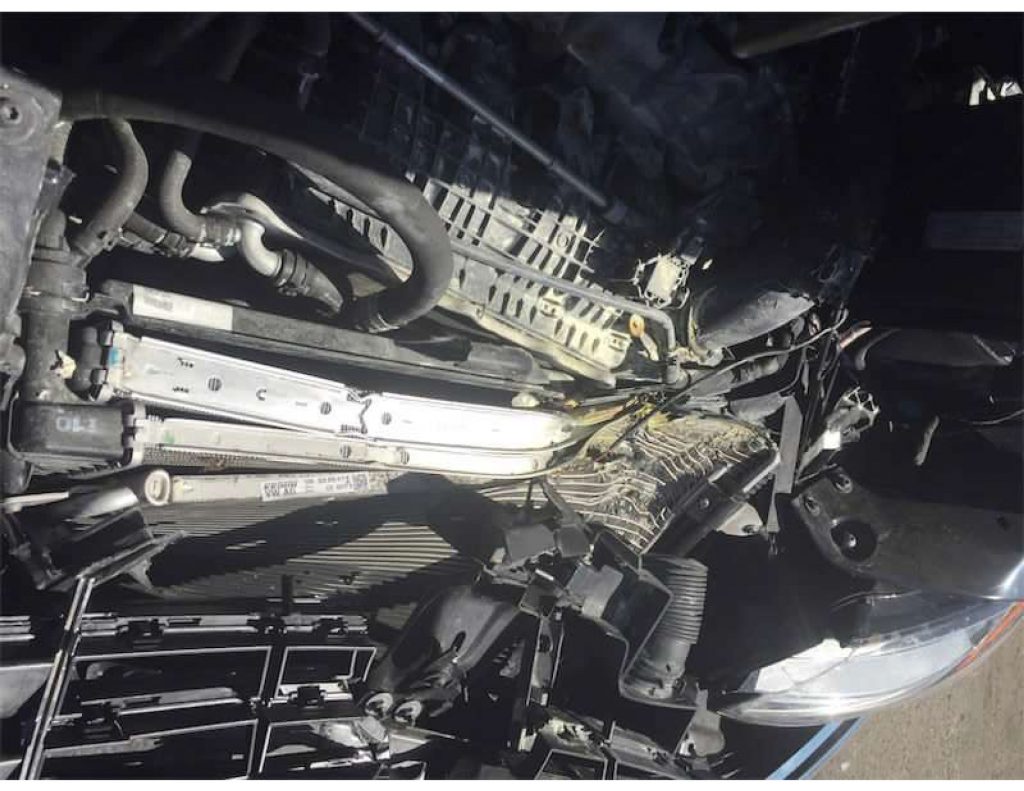
27 million car accidents have occurred, 171,000 people have died since my accident 7-27-2019. I am grateful to live, but living in a body with a pain level 6-8 out of 10, 24/7 has tested my choice to continue. It has been horrendous to keep going, to keep my place, care for my horses. dogs, myself, and observe losses I never envisioned. What kind of person can afford to get well when health care only covers medication and not the actual recovery process? Not to mention the stress over loss of clients and so much more since brain and body pain/function was severely altered. I’ll cover this topic in the future – as justice too long delayed is justice denied.
To counter this, I dove into research to find questions and answers. To say I am astounded at my findings is an understatement! Up until 7-26-2019, I was completing the education for what I considered my final practitioner certification program… Two courses left. I couldn’t have anticipated the education level the car accident injuries gifted me. I studied and earned at least 3 alternative Phd’s… (Kidding, but seriously…)
Soft tissue injuries are as complicated as it gets… medication, surgery, are deemed not current solutions to these injuries. Those people who laugh at or dismiss soft tissue damage and pain as ‘not real’ or ‘psychological’, are dwindling. New testing is uncovering a whole new level of understanding and resolution to what was terminal illness. Current research is astounding, findings are complex, simple, self treatable and treatable via specialists. Knowledge is the success for our present day and our future. Seek out help from those who stay current.
“There are a lot of politics that keep the drug companies well staffed and well-funded that keep the system as it is. Those with a medical license have to abide by things that are ‘evidence based’ which is studies of 5000 or more with consistent results. Some people show success with hyperbaric oxygen therapy, chiropractic, craniosacral and some don’t. Some people show success with medication and some don’t.” So, the money fuels the requirements of the system that our insurance supports therefore the evidence based studies are medication-based. Current research time and again says medication is a temporary pacifier until self healing typically occurs. Studies on long term use of medication used in brain injuries show detrimental effects, and leave a patient in more pain than they would be in had they not taken medication.
Current study test results show what is most beneficial for healing to take place is proper nutrition, supplements that benefit the brain and body which are recommended after testing, addressing inflammation, proper amount of sleep, exercise specific to injury recovery, stress reduction at all costs, along with support from family, friends, work environment, caregivers that are educated on recovery needs and support. All this not supported by insurance or med pay coverage.
The test offered to me was an MRI for my brain not an fMRI. Studies show 80% of traumatic brain injury MRI test results are absolutely clear of brain bleeds and blood flow complete blockage. Ruling this out is not helpful when it comes to brain function. What happens with brain injuries has to do more with the nervous system, neurotransmitters, than actual brain bleeds. Even blood brain barrier breach is not shown on an MRI, yet the majority of people with traumatic brain injuries have blood brain barrier breach as well as heart issues that develop.
You… I… are the ones who know what we are feeling, experiencing, and with descriptions, terminology along with self tests – what is going on can be determined without a doctors degree. Why do I say this? Just one example: A neuroscience and spine institute – Physical Medicine and Research doctor asked me to describe my pain… I tried desperately to be specific. The doctor listened, finally stated “I am waiting to hear in my terminology what you are experiencing”.
I am a highly educated equine practitioner – my patients – horses and dogs – don’t ‘tell’ me in English what is wrong – I see & feel it based on tiny responses they show me, I then realign and correct their response – the issue is gone…
Regardless, I answered the doctor in her terms, and was given a nerve test. #8 on the diagnosis nailed it – but the diagnoses doctor stated the test was within normal limits. Stabbing pain is not normal, IMO. A year later I experienced extreme sciatic nerve pain – L4-5… When I finally googled #8 on the nerve test – the answer was “this points to compressed or pinched nerve at L4-5”. Great… Specific exercises could have avoided the progression . I accepted an epidural which lasted 15 days, only 4 per year @ $2,000 each can be administered. Not a viable solution, waste of valuable time. So I found a simple permanent solution myself.
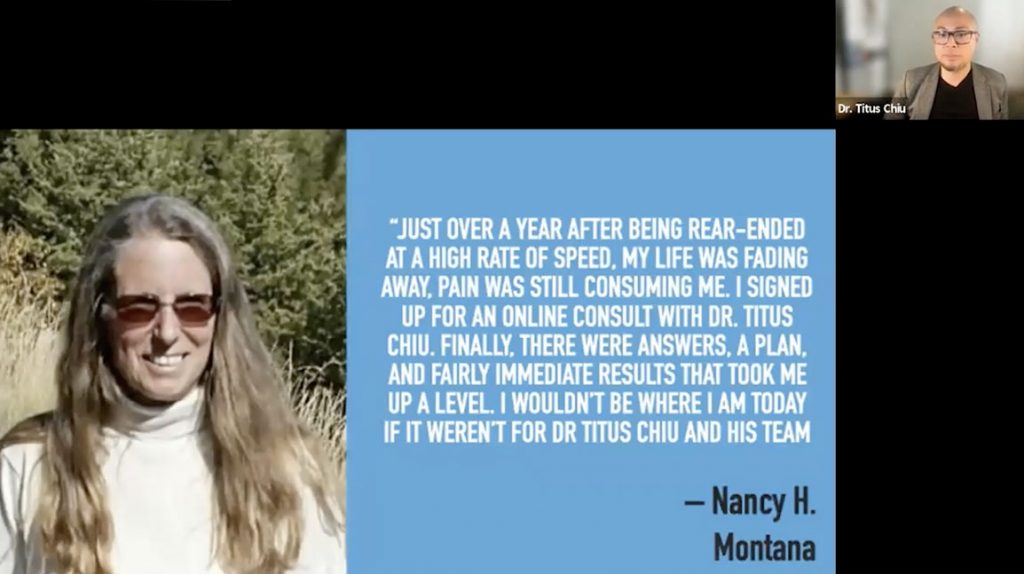
I patiently waited for the one year mark – not better, in fact worse. I was lucky enough to find a functional neurologist offering education, self testing and answers. The first of 3 intensive programs… Stay tuned for more.